“Things get done only if the data we gather can inform and inspire those in a position to make a difference.” – Mike Schmoker, former school administrator, English teacher and football coach, author.
In the first of our series of articles about the foundations of an effective population health management program, from a technology perspective, we discussed the six verticals of “The Population Health Management Framework”, identified by KLAS. There we addressed vertical one, Data Aggregation and its importance. The verticals identified by KLAS are commonly accepted in the healthcare industry as the necessary components to build the technical foundation to transition from a fee-for-service world to value-based care.
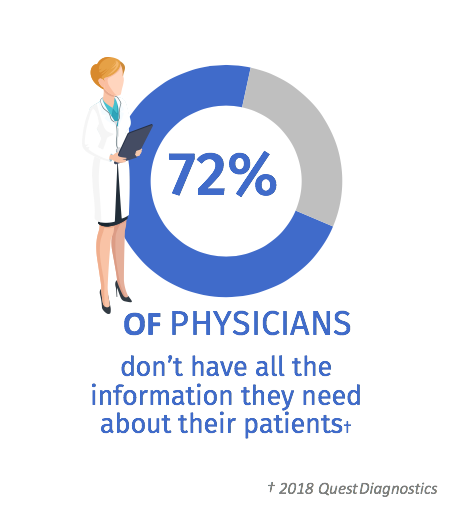
In this second article, we will discuss vertical two, Data Analysis. Data analysis builds on vertical one, Data Aggregation. Once the data is aggregated from disparate sources, such as billing, claims, EMR systems, tertiary health systems, financial systems, patient satisfaction systems, clinical systems such as labs, rad, transcriptions, etc., and other data sources, it needs to be compiled together, and organized into a cross-functional data warehouse across patient populations. KLAS defines this vertical as, “automated tools to stratify a population across risk factors and to facilitate communication through reports, benchmarking, and predictive analytics”. Regardless of the type of organization (such as a health plan, ACO, HIE, or IDN), robust data must be collected and organized in such a way that it is useful in population health management activities. In a recent Quest Diagnostics study, they found that 72% of physicians do not have the information they need about their patients. This study illustrates that data remains a challenge for most, mainly constrained by the time, cost, and reliablility of traditional methods.
Here at Holon Solutions, we believe technology will play a vital role in enabling this transition towards value-based care, by breaking down data silos to empower all consumers of healthcare to make the right decisions at the right time. Renee Broadbent, Senior Vice President of Population Health at Holon, and I have continued to strategize around these verticals so that we can ensure our apps at Holon are exceeding the needs of our clients and ensuring their success in the transition to value-based care.
Renee Broadbent:
In managing complex risk-based organizations, there is a need for meaningful and rich data to facilitate successful population health management programs. Good analytics should consider compliance with best practices and whether care is being provided in the most effective and safest way. Spending time acquiring the various data sources, then integrating them into rich cross-functional data models is critical to help manage patient populations. Interestingly, the data, depending on the source, could be in varying forms of ‘usefulness’ and therefore proper data-driven strategies need to be devised to both extract the usable information from the data and then turn the information into actionable insights for all the participating entities, while creating a singular concrete picture of every patient’s health outcomes.
While in my role as a member of an ACO leadership team, once we concluded that our data was in a state that made it accessible and usable by others, we then took to analyzing the information that was available. Our initial focus was on care and coding gaps and how to address those with our constituents. This first step is critical to ensuring quality metrics and other measures are met and the programs are in compliance with specific goals as it impacts revenue and incentive payments. Taking the data, and then transforming it into meaningful reporting, providing curated information to our physicians so that they could make impactful improvements to their workflow, gain efficiencies, meet metrics, but most importantly improve their patients’ outcomes.
As we perfected our data and our scores, and outcomes improved, we started to look more closely at the data, and think: what could it show us for the future? Simply put; what predictive analytics could be derived from it to help better manage populations? We started utilizing our analytics tool to start doing models and then charting populations. We could then place patients in quadrants spanning from healthy to chronically ill. Why is this important? Because the costliest patients to treat are often in the top 5% and resources to help them, limited. The analysis helped us focus our efforts, so we could help the physician identify those patients, improve treatment and drive down cost while improving quality.
The process of data analysis as a core pillar of population health is imperative for facilitating risk-based programs. Curating meaningful, rich, timely insights from the data across their ecosystems (clinical, claims, social determinants of health, patient reported outcomes, and more) helps organizations to thrive in this transition.
Saurabh Mathur:
Data analysis in population health management serves as the backbone of decision making, measuring performance of organizations and individuals towards meeting value-based care goals. If it is done right, the framework for data analysis establishes a model for an operational tripod made up of:
- Defining What Matters – Establishment of best practices and shared baselines for providers to provide cost effective quality care to their patient populations.
- Measuring What Matters – Effective measurement of individual and organization performance through rich data acquisition, and to timely deliver specific, actionable interventions at the point of care.
- Improving upon What Matters – Efficient adoption of mutually agreed upon improvement strategies by providers and organizations to improve care quality, outcomes, patient safety, and reduce waste.
Working in partnership with a strong analytics vendor, a population management organization must build a knowledge base and sets of care improvement guidelines for different disease conditions and comorbidities. The improvement guidelines must incorporate standardized measures, defining key metrics and use historical data to segregate populations of patients needing care improvement opportunities. The standardized measures must be representable as actionable visual insights for care providers and organizations to consume.
Aggregating detailed EMR chart data is a critical piece to establish care improvement guidelines and Holon’s CollaborNet™️ Connect extracts historical patient chart data from EMR systems that can be used to facilitate segregation of patient populations and the associated gaps in patients care or opportunities of care improvements. Using our proprietary methods, we can offer our customers the ability to extend this capability across their network – as it is an affordable option, not reliant on traditional point-to-point interfaces. We Liberate the Data.
When implementing the data analysis systems, while the core capabilities of measuring are defined as part of the properly designed data warehouses, pre-analytics of data at the source contributing systems such as EMRs is critical to ensure quality data aggregation. Here are how two of our apps work together:
- CollaborNet Connect automatically shares clinical data between providers, health plans, and analytics engines. Holon’s proprietary retrieval methodology involves standardinzing the information for data quality and for analytics consumption.
- CollaborNet Insights surfaces real-time, interactive, contextual data at the point of care.
- When deployed together, our dual solutions–Insights and Connect–offer a win-win solution. Insights supplies providers automatic, patient-specific information directly into their EMR at the point of care, making their job easier and their treatment more effective. Connect collects real-time information providers are entering into their EMR and delivers it upstream, providing a wider scope of data to aid in risk management and population health.
Depending upon the maturity of the participating organizations, the adoption of care improvements and guidelines takes a phased approach. In our experience rather than enforcing strict guidelines, a focused approach of reducing care variations and working with the providers to establish best guidelines works better. The key lies in identifying evidence-based guidelines along with suggested improvements for each organization and working together in reducing the variations from those guidelines.
Data analysis is a key component for any organizations creating and managing a population health management program. Without effective data analysis, organizations cannot understand the populations they are managing and develop the programs necessary to achieve improvements in patient care, drive quality scores and impact reimbursement. Holon enables our value-based care partners to solve the pillar of data analysis by curating data from many sources, then using it to enrich the data the client has in their analytics system for even more meaningful data and complete picture of a given population. Holon offers a first-to-market seamless integration, vendor agnostic approach, reliant on our proprietary methods with our point of care platform. Contact us and let us know how we can help you Liberate the Data. Framework Source: KLAS Population Health Management 2017, Part 1 – Validating the adoption of PHMFunctionality


